Antimicrobial resistance (AMR) poses a major threat to human health around the world. Studies show that low- and middle-income countries (LMICs), particularly in South Asia and sub-Saharan Africa, often face the highest rates of mortality associated with bacterial resistance, despite some having lower overall antibiotic consumption rates than the very top-consuming countries in the Middle East.
- Murray, C. J. L., et al. (2022). Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet, 399(10325), 629–655.
- Godman, B., et al. (2022). Tackling antimicrobial resistance across sub-Saharan Africa: current challenges and implications for the future. Expert Opinion on Drug Safety, 21(11), 1435–1448.
Does this then mean that antibiotics might not be the leading cause of superbugs?
No. They are.
The catastrophic mortality rate found in the studies is called the Fatal Gap: the chasm between a patient contracting a resistant infection and receiving a last-resort drug. In the wealthy hyper-consuming nations, a patient might receive three or four lines of increasingly powerful antibiotics, allowing the drug-resistant pathogen to be killed and the patient often survives. In the “Global South”, however, the system fails at the diagnosis and access stage. The patient might have a severe bloodstream infection, but the local lab lacks the diagnostics to identify the resistance profile. When cheap, first-line antibiotics fail, the patient’s fate is sealed because the most effective “last-line” treatments are either nonexistent or too expensive, or simply unknown to the overstretched physician. Thus, the cause of death isn’t the birth of the superbug via antibiotic misuse—it is the systemic, fatal lack of a counter-weapon. The studies confirmed this grim truth: resistance alone was manageable; resistance compounded by the absence of clean water and effective healthcare are a death sentence.
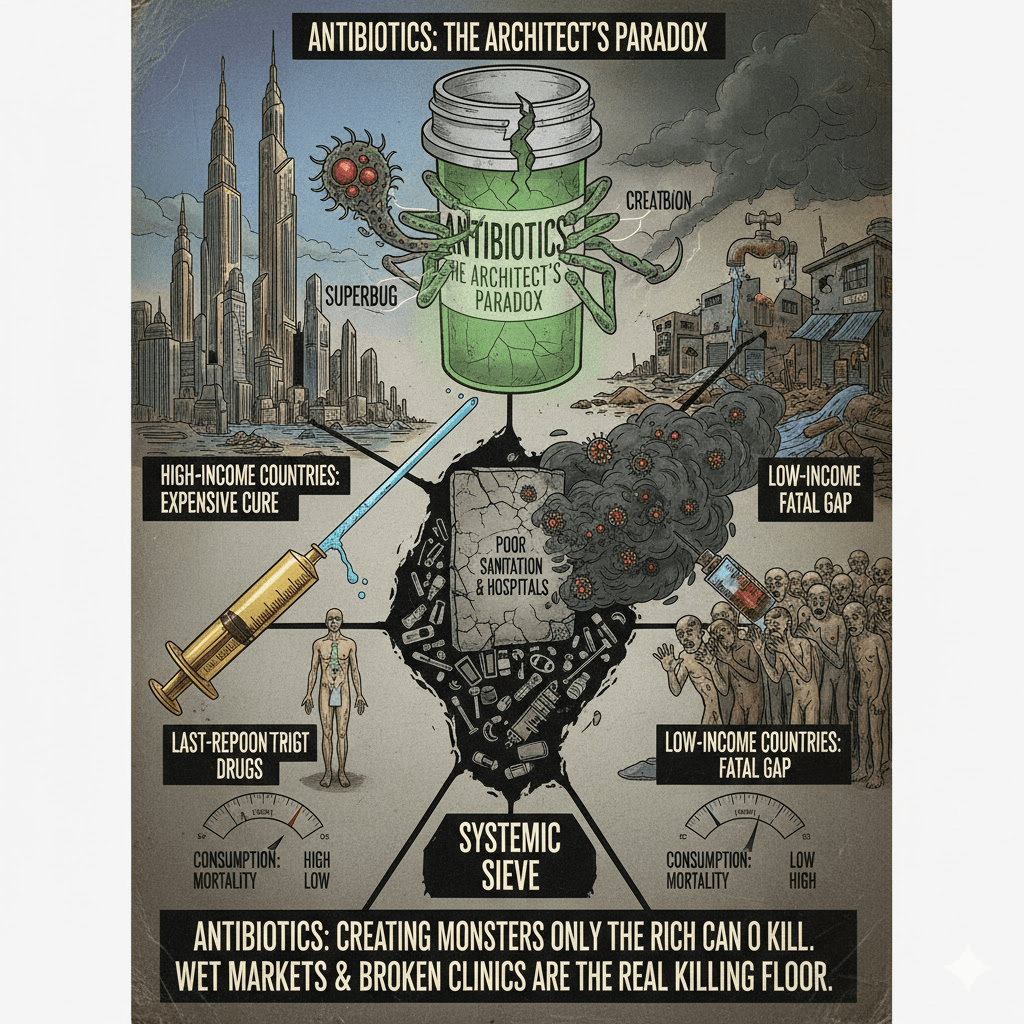
So it is a paradox. Antibiotics may be the leading cause of creating the superbugs, but the same (yet stronger) antibiotics are then required to effectively kill the superbugs. And we keep on looking for better ones, while bacterias adjust. It is a never-ending cycle. Only rich countries can afford this. In low income countries, the consumption of antibiotics is lower, because there are multiple systemic failures to heal someone, who contracted a superbug. And compounded by poor sanitation, poor infrastructure, poor training of physicians, etc.
The global superbug crisis boils down to a tragic joke: Antibiotics are like a necessary addiction that creates its own monster, but only the rich can afford the increasingly expensive recovery program. In low-income countries, they often can’t even afford the starter drug, yet they die at the highest rates because their poor sanitation is a free breeding ground for the monster, and they have no hope of affording the cure (and many of these super bugs travel through “recycled” garbage from the rich countries, which are dumped there). The world needs to worry less about who is popping the most pills and more about who can’t afford a toilet and a life-saving shot (and has to look at all the garbage we produce; garbage that pollute water, food and also bring in “guests” – the superbugs).
So next time you think on it – as per usual – the choice is yours!
Inspired by this article: https://www.visualcapitalist.com/top-35-countries-by-antibiotic-use-see-u-s-ranks/
Leave a comment